Abstract
Background
T-cell lymphoma (TCL) consists of a group of rare and usually aggressive, fast-growing Non-Hodgkin Lymphoma (NHL) that develop from T-cells. Most TCL are Peripheral T-cell lymphoma (PTCL). Central nervous system relapse is a rare but fatal complication of patients with PTCL. Several studies have identified risk factors for CNS relapse in PTCL patients, such as elevated serum lactate dehydrogenase (LDH), >1 extranodal sites of involvement, high International Prognostic Index (IPI) score and specific histological subtypes.
Aim
To investigate risk factors for CNS relapse in PTCL patients including absolute lymphocytes count (ALC) and lymphcytes percent at time of diagnosis.
Methods
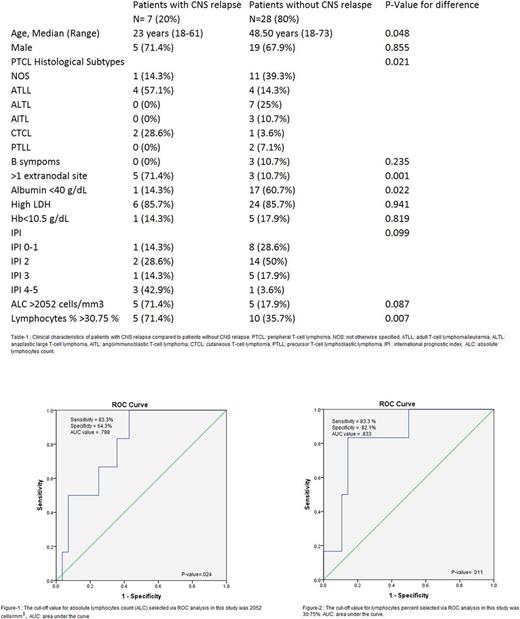
35 patients diagnosed with PTCL between January 2003 and December 2016 at King Abdullah University Hospital (KAUH) were retrospectively reviewed including: 12 not otherwise specified (NOS), 8 adult T-cell leukemia/lymphoma (ATLL), 7 anaplastic large cell lymphoma (ALCL), 3 angoimmunoblastic T-cell lymphoma (AITL), 3 cutaneous T-cell lymphoma (CTCL) and 2 precursor T-cell lymphoblastic lymphoma (PTLL). Clinical and laboratory data at time of diagnosis including gender, age, presenting symptoms, lactate dehydrogenase level (LDH), hemoglobin level (Hb), complete blood count (CBC), lymphocyte percent, albumin level ,pathological subtypes and CT and PET/CT scans were studied. patients followed-up and CNS relapses was confirmed by cerebrospinal fluid (CSF) analysis or histopathological studies. Patients with CNS involvement at diagnosis were excluded from the study. All patients received the same CHOP treatment regimen. None of our patients received prophylactic intrathecal chemotherapy.The optimal cut-off value for ALC and lymphocytes percent was obtained using the Receiver Operating Curve (ROC) with a determination of the sensitivity and specificity .
Results
Among 265 patients diagnosed with NHL, only 35 patients (13.21%) confirmed to have PTCL. 24 patients (68.6%) were males and 11 patients (31.4%) were females. 7 patients (20%) had CNS relapse during the follow-up period. Patient characteristics are summarized in the table. There was significant association between CNS involvement and PTCL subtypes (P-value=.021), involvement of more than one extra-nodal site (P-value=.001) and albumin serum level <40 g/L (P-value=.022) too. The mean age (32.86 years) of patients with CNS relapse was significantly lower than the mean age (45.96 years) of patient without CNS relapse (P-value=.048). Median lymphocytes percent was 25% (range , 7.6%-92%) and the optimal cutoff value of lymphocytes % for predicting CNS relapse risk was 30.75 % (Sensitivity 83.3% , Specificity 82.10%; area under the curve [AUC] value: 0.833, 95% confidence interval [CI] 0.637-.994 , P-value = 0.011). In univariate analysis, High lymphocytes percent was significantly associated with CNS relapse (P-value=0.007). Median ALC was 1840 cells/mm3 (range , 340 cells/mm3 -10500 cells/mm3) and the optimal cutoff value of ALC for predicting CNS relapse risk was 2052 cells/mm3 (Sensitivity 83.3% , Specificity 64.3%; area under the curve [AUC] value: 0.798, 95% confidence interval [CI] 0.633-.962, P -value = 0.024). In univariate analysis, ALC higher than 2052 cells/mm3 wasn't significantly associated with CNS relapse (P-value=0.087). In multivariate analysis, CNS relapse was significantly associated with more than one extra-nodal site involvement (P-value=.001), ALC higher than 2052 cells/mm3 (P-value=.033), lymphocytes % higher than 30.75 (P-value=.001) and albumin serum level <40 g/L (P-value=.04). There was no significant association between CNS relapse and IPI score (P-value=.099) , PIT score (P-value= .076) and B-symptoms (P-value=.235).
Summary
Risk factors for CNS relapses in patients with PTCL at our medical center include : Adult T-cell lymphoblastic lymphoma (ATLL ) and cutaneous T-cell lymphoma (CTCL) subtypes , more than one extranodal site involvement and low serum albumin level at time of diagnosis. Absolute lymphocyte counts higher than 2052 cells/mm3 and Lymphocyte percent higher than 30.75 % at time of diagnosis can be used to predict CNS relapse risk. Identification of CNS relapse risk factors will help in targeting high-risk patients who will benefit from intrathecal chemotherapy prophylaxis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal